Table of Contents - Hot Tub Folliculitis: The Complete Owner’s Guide to Prevention and Treatment
- The Culprit: Pseudomonas Aeruginosa Bacteria
- How You Get Hot Tub Folliculitis
- Hot Tub Folliculitis vs Other Rashes
- Hot Tub Folliculitis Symptoms and Diagnosis
- How to Treat Hot Tub Folliculitis
- The Hot Tub Owner’s Action Plan: Prevention and Decontamination
- Advanced Topics and Misconceptions
- Enjoy Your Hot Tub Safely and Worry-Free
- Frequently Asked Questions
- What is the fastest way to get rid of hot tub folliculitis
- How long after being in a hot tub does folliculitis appear
- Should I pop the pimples from hot tub folliculitis
- Can you get hot tub folliculitis on your face or scalp
- Is hot tub folliculitis a sign of a dirty hot tub
- Will swimming in a chlorinated pool clear up hot tub folliculitis
- Can I go in my hot tub if I have folliculitis
- What’s the difference between hot tub rash and hot tub lung
This blog post may contain affiliate links. As an Amazon Associate I earn from qualifying purchases.
Soaking in a hot tub should be a relaxing escape, not an itchy, painful experience. Yet thousands of hot tub users each year develop hot tub folliculitis, a stubborn bacterial skin infection that can turn your wellness retreat into a medical concern. This comprehensive guide brings together expert dermatological insights, CDC guidelines, and real-world hot tub maintenance strategies to help you understand, treat, and most importantly, prevent this common yet entirely avoidable condition. Whether you’re dealing with an active outbreak or simply want to ensure your hot tub remains a safe sanctuary, this article provides everything you need to know.
- ENERGY-EFFICIENT CONSTRUCTION: EnergySense insulated walls and cover are up to 40% more energy-efficient than similar hot tubs; MaxHold fabric internal beams provide superior air pressure retention, stability and lightweight portability; Tritech 3-layer external material offers superior durability and puncture resistance
- CONTROL WITH YOUR SMARTPHONE: Compatible with the Bestway Connect app that allows you to control the temperature, timer, filter and AirJet massage system; Includes a multi-function pump, which also inflates the hot tub, controls the heat setting (up to 40ºC/104ºF), and runs the filtration system
- STAYS UP ALL YEAR LONG: Freeze Shield protects the pump and liner from damage due to cold weather; The Power-Saving Timer allows you to control the temperature of the water up to 40 days in advance
- PERFECT FOR 7 PEOPLE: 85 in. x 28 in. (2.16 m x 71 cm) hot tub is the perfect size for up to 7 adults, with a water capacity of 314 gal. (1,190 L)
- EVERYTHING YOU NEED: Set includes 1 hot tub, 1 cover, 1 pump, 1 filter cartridge (IV), 1 ChemConnect chemical dispenser, 1 repair patch
- Soothing Airjet Massage System: The Bestway Saluspa Cancun hot tub features 120 bubble jets that create a warm and relaxing spa experience for up to 4 people, right from the comfort of your home.
- Energy-Efficient Design: Insulated walls and cover are up to 40% more energy-efficient in keeping your hot tub warmer, compared to similar hot tubs. NOTE: APSP-14 and Title 20 compliant.This model meets all energy efficiency conditions required for sale in the following states: CA, HI, OR, RI, MA, NJ, ME, NY, NV, MD, WA, D.C.
- Durable Construction: MaxHold fabric internal beams provide superior air pressure retention, stability and lightweight portability. Surrounded by a 3-layer Tritech outer layer, this hot tub is proven to be puncture- and damage-resistant.
- Stays Up All Year Long: Freeze Shield protects the pump and liner from damage due to cold weather. The Power-Saving Timer allows you to control the temperature of the water up to 40 days in advance.
- Convenient Features: Equipped with a pump that quickly inflates the hot tub and an easy-to-reach digital control panel to heat water up to 104˚F (40˚C). ChemConnect dispenser maintains clean, clear water by evenly dispersing the proper amount of chlorine.
- SOOTHING MASSAGE SYSTEM: The SaluSpa Miami Inflatable Hot Tub Spa features 120 jets which release air bubbles to create a warm, relaxing experience at your home! The massage system has two different intensity levels for your preference.
- CONTROL AT YOUR FINGERTIPS: Control this spa from your smart device! Through the Bestway Smart Hub app, you can adjust the water temperature, activate the Power Saving Timer, run the water filter and control the AirJet system. Inside the tub, use the digital control panel to manage the spa’s settings.
- 40% MORE ENERGY EFFICIENT: The specially constructed EnergySense insulated cover is 40% more energy efficient than similar inflatable spas. The cover prevents debris from collecting and retains heat more efficiently, meaning the water stays hotter and your energy bill stays lower.
- DURABLE CONSTRUCTION: The inflatable walls are made of durable, puncture-resistant DuraPlus material which is more tear-resistant and stretch-resistant compared to PVC. The portable spa will retain its shape no matter how many times it’s inflated and deflated. FreezeShiled technology automatically prevents the spa’s inner components from freezing at colder temperatures.
- NOTE: APSP-14 and Title 20 compliant. This model meets all energy efficiency conditions required for sale in the following states: CA, OR, RI, MA, NJ, ME, NY, NV, MD, WA, D.C.
- FIBER-TECH BEAM CONSTRUCTION – Innovative Fiber-Tech Technology offers superior structural stability while maintaining a comfortable surface for a luxorious and refreshing spa experience
- THE ULTIMATE SPA EXPERIENCE – Control all Spa functions from your phone or tablet; program Spa use and maintenance remotely with WIFI connectivity; available on App Store and Google Play App
- REMOVABLE WIRELESS CONTROL PANEL – The Greystone Deluxe PureSpa includes a removable wireless control panel that features integrated wireless charging; 48 hours of operation on a single charge and conveniently attaches to top of the tub
- PREMIUM ACCESSORIES – Everything you need for pure relaxation! Let your worries bubble away with 2 contoured headrests, an energy efficient spa cover, and a mood-setting multi-colored LED light (requires 3 AAA batteries, not included)
- BUILT-IN FASTFILL INFLATION SYSTEM – Designed with a convenient FastFill inflation system; just simply inflate and deflate at a touch of a button, no external hose needed; Inner Dimensions: 49 x 49 x 28 inches; Outer Dimensions: 69 x 69 x 28 inches; Total Length w/ Pump: 88″
- FIBER-TECH BEAM CONSTRUCTION – Innovative Fiber-Tech Technology offers superior structural stability while maintaining a comfortable surface for a luxurious and refreshing spa experience
- HARD WATER TREATMENT SYSTEM – Built-in Hard Water Treatment System makes water gentler on skin, clothes and the entire spa system
- HEATED AIR BUBBLE TECHNOLOGY – The Positive Temperature Coefficient (PTC) heater is designed to maximize heat transfer to the water, while ensuring the highest level of safety, performance, and longevity
- ENERGY EFFICIENT SPA COVER – High density thermal-resistant foam provides extra insulation and minimizes heat loss; this cover enhances the Spa performance while improving the energy efficiency by as much as 50%
- SPECS – Designed to fit up to 4 people; outer dimensions: 77″ x 28″ and inner dimensions: 57″ x 28″; water capacity of 210 gallons; water temperature range: 68-104 degrees Fahrenheit
What is Hot Tub Folliculitis
Hot tub folliculitis is a bacterial skin infection that targets your hair follicles, creating an uncomfortable rash that typically appears within 12 to 48 hours after exposure to contaminated water. Also known as Pseudomonas folliculitis or spa pool dermatitis, this condition manifests as itchy, red bumps that can develop into pus-filled blisters resembling acne. Despite its name suggesting exclusivity to hot tubs, this infection can occur in any inadequately sanitized warm water environment including spas, whirlpools, and even swimming pools.
The infection occurs when bacteria penetrate the outer layer of your skin and infect the hair follicles, those tiny pockets from which each hair grows. Unlike simple skin irritation that might clear up in hours, hot tub folliculitis represents an actual bacterial colonization that requires specific treatment and prevention strategies.
What makes this condition particularly frustrating for hot tub owners is that it serves as a visible indicator of water quality issues. When someone develops folliculitis after using your spa, it’s a clear sign that sanitizer levels have dropped below effective thresholds or that pH balance has drifted outside the safe range.
The Culprit: Pseudomonas Aeruginosa Bacteria
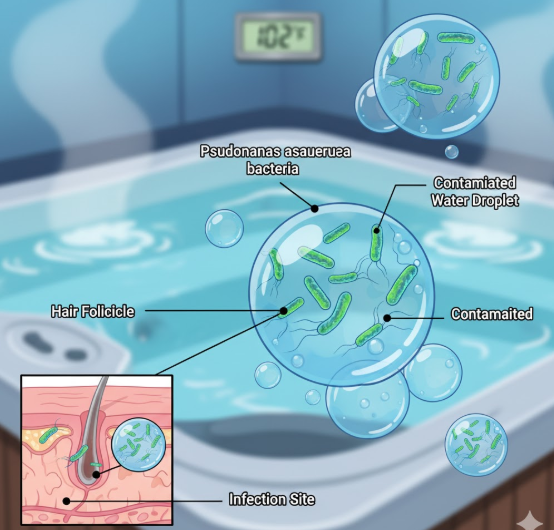
Pseudomonas aeruginosa is the bacterial villain behind hot tub folliculitis, and understanding this microorganism helps explain why this condition is so closely tied to water maintenance. This gram-negative bacterium is naturally present in many environments including soil, water, and even on human skin in small, harmless quantities. However, it becomes problematic when it finds its ideal breeding ground in warm, poorly sanitized water.
Pseudomonas aeruginosa thrives in temperatures between 98 and 104 degrees Fahrenheit, precisely the range most hot tub owners prefer for comfortable soaking. This isn’t coincidental. The bacterium has evolved to flourish in warm, moist environments where it can multiply rapidly when given the opportunity.
What makes this bacteria particularly troublesome for hot tub owners is its relative resistance to standard sanitizer levels. While proper chlorine or bromine concentrations will eliminate it, Pseudomonas can survive in water with marginal or fluctuating sanitizer levels that might control other organisms. The bacterium also forms protective biofilms on surfaces and within plumbing systems, creating reservoirs that continually reseed the water with bacteria even after shocking.
According to the Centers for Disease Control and Prevention, outbreaks of hot tub folliculitis have been linked to both residential and commercial facilities, with the common denominator being inadequate disinfectant levels or improper pH balance that renders sanitizers ineffective. The bacterium’s ability to colonize filters, jets, and plumbing means that surface-level treatment often proves insufficient without addressing the entire water system.
How You Get Hot Tub Folliculitis
The infection pathway for hot tub folliculitis is straightforward but requires specific conditions to occur. When you immerse yourself in contaminated water, particularly for extended periods, the warm water causes your skin pores and hair follicles to open and soften. This natural response, which normally feels pleasant during a soak, creates an opportunity for Pseudomonas bacteria to penetrate the follicle opening.
The bacteria don’t simply float past your skin. Prolonged exposure allows them to establish colonization within the follicle structure, where they trigger an inflammatory immune response. Your body recognizes the bacterial invasion and sends white blood cells to fight the infection, creating the characteristic red bumps and pustules.
Areas covered by swimwear are particularly vulnerable because wet fabric traps contaminated water against your skin, maintaining prolonged contact even as you move around in the tub. This “bathing suit distribution” of the rash is so characteristic that dermatologists often use it as a diagnostic clue. The snug fit of most swimwear combined with areas where friction occurs creates the perfect storm for bacterial penetration.
Minor skin damage also plays a role. Small nicks from shaving, existing skin conditions, or even vigorous scrubbing before entering the hot tub can create entry points that make infection easier. This is why some people develop folliculitis after a single exposure while others who use the same contaminated water might escape infection, though continued exposure significantly increases everyone’s risk.
The concentration of bacteria in the water matters tremendously. A hot tub with marginally low chlorine might have bacterial levels that require a 30-minute soak to cause infection, while severely contaminated water could trigger folliculitis in just 10 minutes of exposure.
Hot Tub Folliculitis vs Other Rashes
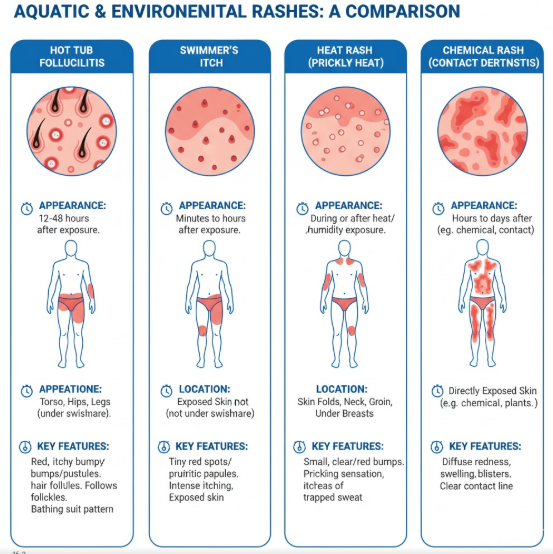
Distinguishing hot tub folliculitis from other skin reactions is essential for proper treatment and prevention. Many hot tub users experience various skin issues that can appear superficially similar, but each has distinct causes, appearances, and treatment approaches. Misidentifying the condition can lead to ineffective treatment and continued exposure to whatever caused the problem in the first place.
Understanding these differences empowers you to take the right action quickly, whether that means adjusting your water chemistry, seeking medical treatment, or simply waiting for a harmless reaction to resolve on its own.
Hot Tub Rash vs Swimmer’s Itch
While both conditions are called “rash” and both relate to recreational water exposure, hot tub rash and swimmer’s itch are fundamentally different problems. Hot tub folliculitis is caused by Pseudomonas bacteria and creates pustules centered on hair follicles, typically in areas covered by swimwear. The bumps are raised, often filled with pus, and appear 12 to 48 hours after exposure.
Swimmer’s itch, medically known as cercarial dermatitis, is caused by parasitic flatworm larvae that burrow into your skin before dying. This creates an allergic reaction that appears as tiny red spots or small raised bumps, typically in areas not covered by swimwear since the larvae in freshwater environments tend to attack exposed skin. Swimmer’s itch appears much faster, often within hours of exposure, and creates intense itching without the characteristic pustules of bacterial folliculitis.
The treatment approaches differ significantly as well. Swimmer’s itch resolves on its own as the dead parasites are absorbed by the body, requiring only symptomatic relief. Hot tub folliculitis may require antibiotics if severe and definitely requires addressing the bacterial source in the water.
Hot Tub Folliculitis vs Heat Rash
Heat rash, or miliaria, occurs when sweat ducts become blocked, trapping perspiration beneath the skin. This creates small, clear or red bumps that are typically very small and not centered on hair follicles. Heat rash commonly appears in skin folds and areas where clothing causes friction, and it develops during or immediately after exposure to heat.
Hot tub folliculitis, by contrast, always centers on hair follicles, develops 12 to 48 hours after water exposure, and creates larger, more pronounced pustules. Heat rash feels prickly or stinging, while folliculitis tends toward deeper pain or tenderness. Perhaps most tellingly, heat rash improves rapidly once you cool down and dry off, while folliculitis persists and may worsen without treatment.
The prevention strategies differ completely. Heat rash prevention focuses on staying cool, wearing breathable fabrics, and keeping skin dry. Folliculitis prevention requires proper water sanitation and chemical balance.
Hot Tub Folliculitis vs Chemical Rash or Irritation
Chemical irritation from excessive chlorine, bromine, or pH imbalance can create a rash that hot tub users sometimes confuse with folliculitis. Chemical burns or irritation appear much more quickly, often during or immediately after exposure to improperly balanced water. The affected areas typically feel like a sunburn with redness, stinging, and sometimes peeling skin, but without the follicle-centered pustules.
High chlorine or bromine levels create a diffuse redness across all exposed skin, not concentrated in hair follicles. Your eyes may burn, your swimsuit might show bleaching or discoloration, and you’ll often notice a strong chemical odor in the water. The rash pattern doesn’t follow the “bathing suit distribution” seen with folliculitis.
Chemical irritation resolves quickly once exposure ends and requires no antibiotic treatment. However, it serves as a warning that your water chemistry needs immediate attention. Interestingly, both chemical irritation and folliculitis can stem from the same root cause: improper water balance. High sanitizer levels cause chemical burns, while low levels invite bacterial growth and folliculitis.
Hot Tub Folliculitis Symptoms and Diagnosis
Recognizing hot tub folliculitis accurately and promptly allows for faster treatment and helps identify the water quality issue before others are exposed. While mild cases may seem like a simple annoyance, understanding when symptoms warrant medical attention can prevent complications and ensure you receive appropriate care. The characteristic presentation of this condition makes it relatively distinctive once you know what to look for.
Proper diagnosis typically combines visual examination with your history of recent hot tub use, creating a clear clinical picture that experienced healthcare providers recognize immediately.
What Does Hot Tub Folliculitis Look Like

Hot tub folliculitis presents as clusters of itchy, red bumps that typically range from 2 to 10 millimeters in diameter. Within 24 to 48 hours of initial appearance, many of these bumps develop into pustules, small pus-filled blisters with a white or yellow center surrounded by an inflamed red base. Each pustule centers on a hair follicle, and if you look closely, you may see the hair shaft emerging from the center of some bumps.
The rash typically appears in a “bathing suit distribution,” meaning it concentrates on the torso, buttocks, thighs, and areas that were covered by swimwear during your hot tub session. Arms, legs, and the trunk are most commonly affected, while the face, hands, and feet are usually spared unless they remained submerged for extended periods.
The skin surrounding the pustules often appears pink or red, and the entire affected area may feel tender to touch. Unlike acne, which develops gradually over days, hot tub folliculitis appears relatively suddenly and affects multiple follicles simultaneously in the exposed area. The pustules may vary in size even within the same outbreak, with some remaining small bumps while others develop into larger, more obvious lesions.
On darker skin tones, the redness may be less apparent, but the raised bumps and pustules remain visible, sometimes appearing as darker spots or hyperpigmented areas around each affected follicle. The texture change is often more noticeable than the color change on melanin-rich skin.
Common Symptoms to Watch For
Beyond the visible rash, hot tub folliculitis creates a constellation of symptoms that help distinguish it from other conditions:
- Intense itching that often worsens at night or when the area becomes warm
- Tenderness or pain when touching the affected area or when clothing rubs against it
- Timing of appearance between 8 hours to 5 days after hot tub use, most commonly within 12 to 48 hours
- Concentration of bumps in areas covered by swimwear, with relatively clear skin in exposed areas
- Pus-filled bumps that may ooze clear or yellowish fluid if they rupture
- Low-grade fever in some cases, typically under 101°F
- General malaise or feeling unwell, though this is less common with localized infections
- Persistence of symptoms beyond a few days without improvement
The severity can range from a few scattered bumps that cause minor annoyance to extensive, painful eruptions covering large portions of the torso and upper legs. Most people fall somewhere in the middle, with several dozen pustules creating significant discomfort but not constituting a medical emergency.
Importantly, symptoms don’t improve significantly within the first 24 to 48 hours without intervention, unlike heat rash or mild chemical irritation which often resolve quickly once exposure ends.
When to See a Doctor
While many cases of hot tub folliculitis resolve with home care, certain situations warrant professional medical evaluation. Seeking timely medical attention can prevent complications, ensure proper diagnosis, and provide relief faster than self-treatment alone.
You should consult a healthcare provider if:
The rash is severe, covering large areas of your body, or the pustules are particularly large or painful. Extensive infections may require prescription antibiotics rather than just topical treatment.
Symptoms persist beyond 7 to 10 days despite appropriate home care measures. This could indicate a resistant bacterial strain or suggest an alternative diagnosis.
You develop fever, chills, or signs of spreading infection such as red streaks extending from the affected area. These symptoms suggest the infection may be entering the bloodstream, requiring immediate medical attention.
The pustules become increasingly painful, swollen, or begin to form larger abscesses. This progression indicates deepening infection that won’t resolve without medical intervention.
You have a compromised immune system due to diabetes, HIV, cancer treatment, or immunosuppressive medications. These conditions increase your risk of complications and may require more aggressive treatment.
You’re unsure whether your rash is actually folliculitis or another condition requiring different treatment. Accurate diagnosis ensures you’re addressing the right problem.
The rash affects your face, which is less common with hot tub folliculitis and may indicate a different condition requiring specific treatment to prevent scarring.
How Doctors Diagnose Pseudomonas Folliculitis
Diagnosis of hot tub folliculitis typically begins with a visual examination of the rash combined with your medical history. A healthcare provider will ask about recent hot tub, spa, or pool use, the timing of symptom onset, and whether others who shared the water have developed similar symptoms.
The characteristic appearance of pustules in a bathing suit distribution combined with appropriate timing after water exposure creates a clinical picture that’s often sufficient for diagnosis. The dermatologist or primary care physician will examine the rash pattern, note the follicle-centered nature of the pustules, and may gently palpate the area to assess tenderness and depth of infection.
In most straightforward cases, no testing is necessary and treatment begins based on clinical diagnosis. However, if the presentation is atypical, the infection is severe, or you haven’t responded to initial treatment, your doctor may take a culture sample. This involves using a sterile swab to collect fluid from a pustule or, less commonly, taking a small skin biopsy from an affected area.
The sample goes to a laboratory where technicians culture it to identify the specific bacteria responsible. Pseudomonas aeruginosa grows readily in culture and can usually be identified within 24 to 48 hours. In cases where the infection proves resistant to standard treatment, antibiotic sensitivity testing can identify which medications will be most effective against your particular bacterial strain.
Dermoscopy, a technique using a specialized magnifying device, may help experienced dermatologists confirm that the bumps are centered on hair follicles, distinguishing folliculitis from other pustular conditions.
How to Treat Hot Tub Folliculitis
Treatment for hot tub folliculitis focuses on eliminating the bacterial infection, managing symptoms like itching and discomfort, and preventing secondary complications such as scarring or deeper skin infections. Most cases resolve with conservative home care, though severe or persistent infections may require medical intervention. The key is starting appropriate treatment early and being consistent with your approach.
Always remember that while these treatments address your symptoms, they don’t prevent recurrence. The contaminated water source must be properly sanitized before anyone uses it again, or reinfection is virtually guaranteed.
Home Remedies and Over-the-Counter Solutions
For mild to moderate hot tub folliculitis, several home care measures can speed healing and provide significant relief while your body’s immune system fights the infection.
Warm compresses are your first line of defense. Soak a clean washcloth in warm, not hot, water and apply it to the affected areas for 10 to 15 minutes, three to four times daily. The warmth increases blood flow to the area, bringing infection-fighting white blood cells while also helping to draw out infection from the pustules. This simple intervention can significantly reduce both discomfort and healing time.
Anti-itch creams containing hydrocortisone (0.5% to 1% strength available over-the-counter) can provide temporary relief from the intense itching that often accompanies folliculitis. Apply a thin layer to affected areas up to four times daily. Calamine lotion offers an alternative that soothes irritated skin without the steroid component, making it suitable for more frequent application.
White vinegar soaks offer mild antiseptic properties that can help reduce bacterial load on the skin surface. Mix one part white vinegar with four parts lukewarm water and soak a clean cloth in this solution, then apply it to affected areas for 10 minutes twice daily. The acidic environment is inhospitable to Pseudomonas while being gentle on your skin. Never apply undiluted vinegar, as this can cause irritation and chemical burns.
Keep the affected area clean and dry. Shower daily with a gentle, fragrance-free cleanser, but avoid harsh scrubbing which can spread bacteria and irritate inflamed follicles. Pat dry thoroughly, especially in skin folds, and wear loose, breathable cotton clothing that doesn’t trap moisture against your skin.
Avoid shaving the affected area until the infection has completely cleared, as shaving can spread bacteria and create new entry points for infection. Similarly, resist the strong temptation to squeeze or pop pustules. This can drive bacteria deeper into the skin, spread infection to adjacent follicles, and significantly increase your risk of permanent scarring.
Over-the-counter antibiotic ointments like those containing bacitracin or neomycin have limited effectiveness against Pseudomonas aeruginosa, which is often resistant to these medications. However, they may help prevent secondary infection from other bacteria if pustules rupture. Apply sparingly and only to broken skin, not to intact pustules.
Oral antihistamines like diphenhydramine or cetirizine can help manage itching, particularly at night when it tends to worsen and can disrupt sleep. Follow package directions and be aware that some formulations cause drowsiness.
Medical Treatments for Hot Tub Folliculitis

When home care proves insufficient or the infection is severe from the onset, medical treatment becomes necessary. Healthcare providers have several prescription options that target Pseudomonas aeruginosa more effectively than over-the-counter remedies.
Topical antibiotics specifically effective against Pseudomonas may be prescribed for localized infections that haven’t spread extensively. These prescription-strength formulations contain antibiotics like gentamicin or tobramycin that can penetrate follicles and eliminate the bacteria. Your doctor will instruct you to apply these medications two to three times daily to all affected areas, typically for 7 to 10 days even if symptoms improve sooner.
Oral antibiotics represent the standard treatment for moderate to severe hot tub folliculitis. Ciprofloxacin is the most commonly prescribed medication because Pseudomonas aeruginosa is typically susceptible to this fluoroquinolone antibiotic. Treatment courses usually run 7 to 14 days depending on severity. According to the American Academy of Dermatology, oral antibiotics significantly shorten the duration of symptoms and reduce the risk of complications.
Alternative oral antibiotics include levofloxacin for patients who cannot tolerate ciprofloxacin, though fluoroquinolones carry specific risks and aren’t appropriate for everyone. Your doctor will consider your medical history, other medications, and any drug allergies when selecting the most appropriate antibiotic.
It’s critical to complete the entire prescribed course of antibiotics even after your symptoms disappear. Stopping early can allow resistant bacteria to survive and multiply, potentially causing a more difficult-to-treat recurrence.
For pain and discomfort, your healthcare provider may recommend prescription-strength anti-inflammatory medications or may confirm that over-the-counter options like ibuprofen or naproxen are appropriate for your situation. These medications reduce inflammation around infected follicles, providing relief while antibiotics work to eliminate the infection.
In rare cases of severe infection with abscess formation, a healthcare provider may need to perform incision and drainage. This minor procedure releases pus from large, painful lesions, providing immediate relief and allowing topical antibiotics better access to the infection site.
How Long Does Hot Tub Folliculitis Last
The duration of hot tub folliculitis varies based on infection severity, your immune system health, and how quickly you begin appropriate treatment. Understanding the typical timeline helps set realistic expectations and alerts you when your healing isn’t progressing as it should.
Mild cases with only a few scattered pustules often resolve on their own within 7 to 10 days without any medical treatment. Your immune system recognizes and fights the infection, gradually clearing bacteria from the follicles. During this time, new pustules may continue to appear for the first 2 to 3 days before the outbreak plateaus and begins resolving.
With proper home care including warm compresses and keeping the area clean, mild to moderate cases typically show noticeable improvement within 3 to 5 days. The intense itching usually subsides first, followed by flattening of the pustules and gradual fading of redness. Complete resolution usually occurs within 7 to 14 days.
When treated with appropriate oral antibiotics, even severe cases typically improve dramatically within 48 to 72 hours of starting medication. The pustules stop forming, existing lesions begin to heal, and discomfort decreases significantly. Full clearance with antibiotics usually occurs within 7 to 10 days, though some residual redness or hyperpigmentation may persist for several weeks as the skin completes its healing process.
Factors that can prolong healing include continued exposure to contaminated water, underlying skin conditions like eczema, compromised immune function, and secondary bacterial infection from scratching or manipulating the pustules. Smoking can also slow healing by reducing blood flow to the skin.
Post-inflammatory hyperpigmentation, where healed pustules leave dark spots on the skin, is common and can last for weeks or even months after the infection has cleared, particularly on darker skin tones. These marks are not an indication of active infection and will gradually fade, though sun protection can help prevent them from darkening further.
If your symptoms haven’t improved within 7 days of starting home treatment, or if you’re getting worse rather than better, medical evaluation is necessary to ensure you’re dealing with uncomplicated folliculitis rather than a more serious condition.
The Hot Tub Owner’s Action Plan: Prevention and Decontamination
Prevention is infinitely preferable to treatment when it comes to hot tub folliculitis. As a hot tub owner, you have complete control over the factors that allow Pseudomonas aeruginosa to flourish and cause infection. This section transforms understanding into action with specific, proven strategies that will keep your hot tub safe for everyone who uses it. These aren’t optional best practices but essential maintenance requirements that separate a safe spa from a bacterial incubator.
The good news is that preventing hot tub folliculitis doesn’t require expensive equipment or complex chemistry knowledge. It does require consistency, attention to detail, and a commitment to regular maintenance that never takes a vacation, even when you do.
Why Your Hot Tub is the Perfect Breeding Ground
Understanding the environmental conditions that Pseudomonas aeruginosa requires helps explain why hot tubs present such a perfect storm for bacterial growth. Your spa’s temperature, typically maintained between 100 and 104 degrees Fahrenheit for comfort, falls squarely within the ideal growth range for this bacterium. While you’re enjoying a relaxing soak, bacteria are reproducing at exponential rates if given the opportunity.
Warm water accelerates the breakdown of sanitizers like chlorine and bromine. What would be an adequate sanitizer level in a 78-degree swimming pool becomes insufficient within hours in a 102-degree hot tub. The elevated temperature increases the chemical reaction rates that neutralize your disinfectants, creating a constantly moving target for water chemistry maintenance.
The aeration from jets, while therapeutic for your muscles, creates additional challenges for water quality. Jets introduce air into the water, and this oxidation process rapidly depletes available chlorine. The turbulence also helps suspend organic matter throughout the water column rather than allowing it to settle or be filtered out. Every time someone enters your hot tub, they introduce organic contaminants including skin cells, oils, cosmetics, and yes, bacteria from their body. This “bather load” immediately begins consuming your sanitizer.
The relatively small water volume of most residential hot tubs means that these contaminants become highly concentrated. A residential spa typically holds 300 to 500 gallons of water, compared to 20,000 gallons or more for a swimming pool. When four people soak in your hot tub for an hour, the concentration of organic matter per gallon becomes remarkably high, placing tremendous demand on your sanitation system.
Biofilms represent another hidden challenge. These slimy bacterial colonies form on surfaces throughout your plumbing system, inside jets, and within filter media. The protective matrix that bacteria create in biofilms makes them up to 1,000 times more resistant to sanitizers than free-floating bacteria. These biofilms continuously shed bacteria into your water, recontamination it even after shocking or adding fresh sanitizer.
Step 1: Master Your Water Chemistry
Water chemistry mastery is not optional for hot tub owners who want to prevent folliculitis and other waterborne illnesses. The chemistry isn’t complicated, but it requires regular attention and a willingness to test and adjust as needed. These aren’t suggestions but requirements backed by CDC guidelines and public health research.
Sanitizer levels represent your primary defense against Pseudomonas aeruginosa and other pathogens. For chlorine-based systems, maintain free chlorine between 3 and 5 parts per million (ppm) at all times, with levels potentially reaching 8 to 10 ppm immediately after shocking. Free chlorine is the active, germ-killing form of chlorine, distinct from combined chlorine or chloramines which have little sanitizing power.
For bromine systems, maintain levels between 4 and 6 ppm, with acceptable ranges extending to 8 ppm. Bromine remains effective at higher pH levels than chlorine and doesn’t produce the same strong odor, making it popular for indoor installations. However, bromine is more expensive and requires consistent monitoring just like chlorine.
Testing your sanitizer level before each use is ideal for frequently-used residential hot tubs. At minimum, test every other day even when the tub isn’t in use, as sanitizer depletes over time from heat and UV exposure even without bathers. Commercial facilities should test multiple times daily, particularly during peak use periods.
pH balance is equally critical because sanitizer effectiveness depends entirely on proper pH. Chlorine’s killing power drops by more than 50% when pH rises above 8.0, even if chlorine concentration remains adequate. The ideal pH range is 7.2 to 7.8, with 7.4 to 7.6 being optimal. At this pH, chlorine works efficiently, bathers remain comfortable, and equipment corrosion is minimized.
Low pH (acidic water) causes equipment corrosion, skin and eye irritation, and rapid sanitizer depletion. High pH (alkaline water) creates cloudy water, scale formation, reduced sanitizer effectiveness, and can promote bacterial growth despite adequate sanitizer concentration. Many hot tub folliculitis outbreaks occur in hot tubs with plenty of chlorine but pH levels above 8.0 that render that chlorine largely ineffective.
Total alkalinity serves as a pH buffer, preventing rapid pH swings. Maintain total alkalinity between 80 and 120 ppm. Proper alkalinity makes pH easier to manage and more stable, reducing the frequency of adjustments needed.
Test your water using reliable test strips or a liquid test kit. Digital testers offer the highest accuracy but require calibration and proper storage. Whatever testing method you choose, follow the instructions precisely and replace test strips before their expiration date, as old strips provide inaccurate results.
For comprehensive guidance on maintaining the electrical components that power your hot tub’s circulation and heating systems, understanding hot tub electrical installation requirements ensures your equipment operates safely and reliably, supporting consistent water quality.
Step 2: The Decontamination Protocol After an Outbreak
If someone has developed hot tub folliculitis after using your spa, you must assume your water is contaminated and take decisive action before anyone uses it again. Half-measures will leave bacterial reservoirs that can cause repeat infections, damaging your reputation and potentially exposing you to liability.
Shocking the water is your first step. This process, also called superchlorination, involves raising free chlorine to 10 to 20 ppm for several hours to kill bacteria throughout the water and in biofilms. For a chlorine system, add 3 to 5 times your normal dose of chlorine shock. For bromine systems, you’ll use a chlorine-based shock as an oxidizer even though bromine is your regular sanitizer.
Turn off the air to your jets to minimize off-gassing, but keep the circulation pump running to ensure the shock treatment reaches all plumbing. Let the elevated chlorine level work for at least 4 to 6 hours, ideally overnight. Test before allowing anyone back in, ensuring levels have dropped back to the safe range of 3 to 5 ppm.
Your filter requires immediate attention because it likely harbors Pseudomonas bacteria within its pleats and fibers. Remove the filter and inspect it carefully. If it shows any signs of deterioration, discoloration, or hasn’t been replaced within the past year, replacement is your safest option.
For filters in good condition, deep cleaning is essential. Rinse thoroughly with a high-pressure nozzle to remove large debris, then soak overnight in a filter-cleaning solution specifically designed to break down oils and organic matter. After soaking, rinse again thoroughly, then soak in a diluted bleach solution (one part household bleach to twenty parts water) for one hour to kill bacteria. Rinse exhaustively to remove all bleach residue before reinstalling.
Understanding the complete process of how to clean a hot tub filter ensures you’re eliminating bacterial reservoirs that can cause reinfection even after shock treatment.
For a confirmed, serious outbreak or if you’ve had repeated folliculitis cases, a complete drain, deep clean, and refill provides the only guarantee that you’ve eliminated the problem. Drain the hot tub completely and scrub the entire shell with a non-abrasive cleaner, paying particular attention to the waterline where biofilm accumulates. Remove and clean all filter cartridges, jets covers if removable, and any other components that contact the water.
Before refilling, use a plumbing system cleaner or purge product. These specialized chemicals circulate through your pipes, breaking down the biofilm that forms inside your plumbing where regular sanitizers can’t reach. Follow the product directions carefully, typically circulating the cleaner through the system for several hours before draining completely.
After draining the purge product, wipe down all accessible surfaces, then refill with fresh water. Balance your chemistry immediately, bringingpH, alkalinity, and sanitizer to proper levels before anyone uses the spa.
Step 3: Long-Term Prevention Strategies

Creating a sustainable maintenance routine prevents bacterial buildup and ensures your hot tub remains safe for continuous use. These practices should become automatic habits for every hot tub owner.
Regular draining and refilling every 3 to 4 months prevents the accumulation of dissolved solids that sanitizers can’t eliminate. Even with perfect chemistry maintenance, organic matter accumulates over time, creating a burden on your sanitization system. Calculate your drain interval using the formula: gallons of water divided by (number of regular users times three), with the result representing days between draining. A 400-gallon hot tub with four regular users should be drained approximately every 33 days, or about monthly.
Shower before entering your hot tub every single time. This simple habit removes oils, lotions, deodorant, cosmetics, hair products, and bacteria from skin before they enter your water. Studies show that a quick shower before soaking can reduce organic contamination by 70% or more, dramatically reducing the burden on your sanitizer and extending time between water changes.
Run your filtration system for the manufacturer’s recommended duration, typically 8 to 12 hours daily for residential hot tubs. This continuous turnover ensures water passes through the filter multiple times daily, removing suspended particles and maintaining consistent sanitizer distribution throughout the spa. Modern hot tubs with efficient pumps cost only pennies per day to run filtration cycles, making this extremely cost-effective prevention.
Avoid overcrowding your hot tub. Manufacturer capacity ratings assume proper water maintenance and limited duration soaks. If you regularly have your hot tub at maximum capacity, test and adjust your chemistry immediately after these heavy-use periods, as sanitizer will be significantly depleted. Consider running an extra filtration cycle and possibly adding additional sanitizer to compensate for the heavy bather load.
Keep a maintenance log documenting your test results, chemical additions, filter cleanings, and drain dates. This record helps you identify patterns, ensures you don’t miss maintenance tasks, and provides valuable documentation if problems do occur. Many hot tub manufacturers now offer apps that simplify this logging process and send maintenance reminders.
Replace your filter according to the manufacturer’s schedule, typically every 12 to 24 months depending on use frequency. A degraded filter cannot effectively remove particles and may harbor bacteria that continuously contaminate your water. Mark your calendar when you install a new filter so you remember the replacement date.
Alternative Sanitizers and Folliculitis Prevention
Hot tub owners have several sanitization options beyond traditional chlorine or bromine, and understanding how these systems work helps you make informed decisions for your specific situation. However, every system ultimately requires some residual sanitizer in the water to maintain protection between equipment cycles.
Saltwater hot tub systems have gained popularity based partly on the misconception that they’re chlorine-free. In reality, saltwater systems use electrolysis to generate chlorine from dissolved salt (sodium chloride). The chlorine produced by the salt cell is chemically identical to chlorine added from a bottle or bucket. The advantages are smoother-feeling water and reduced need to manually add chlorine, but you still must monitor free chlorine levels and maintain proper pH balance. The same chemistry rules apply because you’re still using chlorine as your sanitizer.
Ozone and UV systems offer powerful secondary sanitation that can significantly reduce your chemical sanitizer needs. Ozone generators produce O3, an unstable molecule that oxidizes and destroys organic contaminants and kills bacteria extremely effectively. UV systems expose water to ultraviolet light that damages bacterial DNA, preventing reproduction and killing microorganisms. Both technologies work only while water flows through the treatment device, providing no residual protection once water returns to the spa.
This is why even with ozone or UV systems, you must maintain a residual sanitizer level of at least 1 to 3 ppm chlorine or bromine in the spa water itself. The ozone or UV handles much of the bacterial killing, allowing lower chemical concentrations than would otherwise be needed, but eliminating residual sanitizer entirely leaves you vulnerable to bacterial contamination during periods when the system isn’t actively running.
Mineral sanitizers use silver, copper, or other metals that have natural antimicrobial properties. These cartridges or floating dispensers slowly release minerals into the water, supplementing your primary sanitizer. Studies show mineral systems can reduce chlorine or bromine requirements by 50% or more while still maintaining effective sanitation. However, minerals alone cannot maintain safe water chemistry. You’ll still need to maintain at least 0.5 to 1 ppm of chlorine or bromine as a backup sanitizer.
The critical takeaway is that no system completely eliminates the need for water chemistry monitoring. Pseudomonas aeruginosa is opportunistic and will exploit any gap in your sanitation coverage. Whatever system you choose, consistent testing and adjustment remain essential to preventing hot tub folliculitis.
Advanced Topics and Misconceptions
Several persistent myths and common questions about hot tub folliculitis deserve detailed answers. Addressing these topics helps you make informed decisions and avoid practices that provide false security while leaving you vulnerable to infection.
Is Hot Tub Folliculitis Contagious
Hot tub folliculitis is not contagious from person to person through casual contact. You cannot catch this infection by touching someone’s rash, sharing towels with someone who has folliculitis, or being in proximity to an infected person outside of contaminated water. The infection requires direct contact between your skin and water containingPseudomonas aeruginosa bacteria.
This distinction is important because it shifts the focus to where it belongs: the contaminated water source. If multiple people develop folliculitis after using the same hot tub, they each contracted it independently from the water, not from each other. However, this scenario clearly indicates a serious water quality problem requiring immediate attention.
The bacteria can theoretically transfer on shared items that remain wet, such as swimsuits, towels, or washcloths used by someone with active infection. However, this transmission route is uncommon because the bacteria require the warm, moist environment of the hair follicle to establish infection. Once fabric dries,Pseudomonas survival drops dramatically.
Nevertheless, if someone in your household has developed hot tub folliculitis, basic hygiene precautions make sense. They should use separate towels until the infection clears, launder their swimsuit in hot water before anyone else wears it, and avoid sharing bath poufs or washcloths that remain damp.
The real contagion risk is that contaminated water will infect other users before the water chemistry problem is identified and corrected. This is why anyone who develops folliculitis should immediately notify the hot tub owner or facility manager, allowing proper decontamination before additional exposures occur.
Can You Get Folliculitis from a Perfectly Clean Hot Tub
This question addresses a concern many conscientious hot tub owners have: can you do everything right and still have someone develop folliculitis? The short answer is that it’s extremely unlikely, bordering on impossible, if your water chemistry is truly maintained within proper parameters.
Pseudomonas aeruginosa cannot survive in water with adequate free chlorine (3 to 5 ppm) or bromine (4 to 6ppm) at properpH (7.2 to 7.8). These levels provide a hostile environment where bacteria die within seconds to minutes of exposure. If you consistently maintain these parameters and verify them through regular testing, the bacterial load in your water will be virtually zero.
The rare exceptions involve individuals with severely compromised immune systems who might develop infection from bacterial counts so low that a healthy person would clear them without issue. People undergoing chemotherapy, organ transplant recipients taking immunosuppressive drugs, or those with advanced HIV might theoretically develop folliculitis from minimal exposure. For these individuals, consulting their physician before using any hot tub or public pool is advisable.
Pre-existing skin damage also theoretically increases susceptibility. Fresh shaving cuts, active eczema, or other breaks in the skin barrier could allow infection from lower bacterial concentrations than intact skin would resist. However, even in these scenarios, properly sanitized water presents minimal risk.
The reality is that when folliculitis cases occur, investigation almost always reveals a water chemistry lapse. Perhaps the pH had drifted to 8.2, reducing chlorine effectiveness even though chlorine concentration appeared adequate. Maybe the sanitizer wasn’t tested for several days, allowing levels to drop below protective thresholds. Or biofilm had accumulated in the plumbing, continuously seeding bacteria into water that looked clear and tested acceptable at the moment someone used it.
This is why consistent, frequent testing matters more than any single test result. Water chemistry is dynamic, constantly changing based on use, temperature, and time. Yesterday’s perfect chemistry doesn’t guarantee today’s safety.
Risks in Public and Rental Hot Tubs

Using hot tubs you don’t personally maintain requires a different risk assessment and some practical precautions. Hotels, gyms, resorts, and rental properties vary enormously in their maintenance standards, and you often have no reliable way to verify their water quality practices.
The “sniff test” can provide some clues, though it requires understanding what you’re smelling. A strong chemical odor around a hot tub or pool doesn’t indicate cleanliness or excess sanitizer. That distinctive “pool smell” actually indicates chloramines, the compounds formed when chlorine reacts with organic contaminants like sweat, urine, and body oils. A properly maintained hot tub with adequate free chlorine and low organic contamination should have minimal odor. A strong smell suggests either very high contamination that has consumed most available chlorine, or high total chlorine with little free chlorine remaining. Neither scenario is good.
Water clarity offers another assessment tool. Cloudy or hazy water is an immediate red flag indicating inadequate filtration, improper chemistry, or high bacterial counts. Never enter cloudy water regardless of what facility staff might claim about recent shocking or chemical addition. Clear water doesn’t guarantee safety, but cloudy water virtually guarantees problems.
Look for visible biofilm or slime on surfaces, particularly at the waterline and around jets. A well-maintained hot tub should have clean surfaces free of slippery deposits. Discolored grout, stained fixtures, or slimy waterlines indicate maintenance neglect that likely extends to water chemistry.
Observe the facility’s maintenance practices if possible. Do staff test the water visibly and regularly? Is there a posted maintenance log showing recent test results and chemical adjustments? Reputable facilities typically display this information as evidence of their diligence. The absence of such documentation doesn’t prove poor maintenance, but its presence offers some reassurance.
For truly cautious travelers, portable water test strips provide definitive information. These strips cost only a few dollars for a bottle and take up minimal space in your luggage. Before entering any questionable hot tub, dip a test strip and verify that chlorine or bromine and pH fall within acceptable ranges. If readings are outside safe parameters, skip that soak regardless of how inviting the water looks.
Time your hot tub use strategically in commercial settings. Heavy use periods deplete sanitizers rapidly, so soaking immediately after the gym’s rush hour or a hotel’s busy evening may expose you to degraded water chemistry before maintenance staff have restocked sanitizer levels. Early morning, after overnight recovery time and presumed maintenance attention, often offers the safest water quality.
Limit your soak duration in unfamiliar hot tubs. The infection risk increases with exposure time, so a 15-minute soak presents lower risk than an hour-long session. Rinse off thoroughly with clean water immediately after exiting any public hot tub, removing residual bacteria before they have time to colonize follicles.
Consider your recent hair removal practices. If you’ve shaved your legs, underarms, or other areas within the past 24 hours, you have microscopic cuts that increase infection susceptibility. Waiting a day or two after shaving before using public hot tubs reduces your risk.
Finally, trust your instincts. If something about a facility’s hot tub gives you pause, whether it’s the appearance, odor, or general facility cleanliness, don’t use it. No soak is worth a week or more of uncomfortable, pustule-covered skin and potential antibiotic treatment.
Being familiar with proper hot tub wiring standards can also give you insight into whether a facility maintains professional standards across all aspects of their spa operation, as electrical safety often correlates with overall maintenance quality.
Enjoy Your Hot Tub Safely and Worry-Free

Hot tub folliculitis represents a completely preventable condition that should never occur in a properly maintained spa. The key insight throughout this comprehensive guide is that this infection serves as a direct indicator of water quality failure, not an inevitable risk of hot tub ownership. When you understand the relationship between water chemistry and bacterial growth, you gain complete control over the safety of your hot tub experience.
The science is straightforward: Pseudomonas aeruginosa cannot survive in water with adequate sanitizer levels at proper pH. Maintaining free chlorine between 3 and 5 ppm or bromine between 4 and 6 ppm, combined with pH between 7.2 and 7.8, creates an environment where this bacterium dies within minutes of entering your water. Consistent testing and adjustment transform these numbers from abstract chemistry into genuine health protection for you, your family, and your guests.
For hot tub owners facing an active outbreak, the path forward combines proper medical treatment with comprehensive water decontamination. While mild cases often resolve with home care in 7 to 10 days, don’t hesitate to seek medical attention for severe symptoms, persistent infections, or if you have any health conditions that compromise your immune system. Simultaneously, shock your water, deep clean or replace your filter, and consider a complete drain and refill to eliminate bacterial reservoirs that standard treatment might miss.
Prevention requires commitment but not complexity. Test your water regularly, maintain proper chemistry consistently, clean your filter on schedule, and drain your hot tub every few months. Encourage everyone to shower before entering, and never let maintenance slide because “the water looks fine.” These simple habits ensure that hot tub folliculitis remains something you read about but never personally experience.
The investment you’ve made in your hot tub should deliver years of relaxation, therapeutic benefit, and social enjoyment. By mastering the fundamental maintenance practices outlined in this guide, you ensure that every soak is not just enjoyable but genuinely safe. Your hot tub can be both a wellness amenity and a source of pride, maintained to standards that would satisfy the most stringent health inspectors.
Take ownership of your water quality, implement these evidence-based practices, and enjoy your hot tub with the confidence that comes from knowing you’ve eliminated the conditions that allow folliculitis to occur.
Frequently Asked Questions
What is the fastest way to get rid of hot tub folliculitis
Mild hot tub folliculitis typically clears within 7 to 10 days with basic home care including warm compresses and keeping the area clean. For faster resolution or severe cases, consult a doctor who can prescribe oral antibiotics like ciprofloxacin that typically improve symptoms within 48 to 72 hours. There is no instant cure, but medical treatment significantly accelerates healing compared to waiting for the infection to resolve on its own.
How long after being in a hot tub does folliculitis appear
Symptoms typically appear between 12 and 48 hours after exposure to contaminated water, though the range can extend from 8 hours to 5 days. Most people notice the first itchy bumps within a day or two of their hot tub session. The timing is consistent enough that if a rash appears within this window after hot tub use, folliculitis should be strongly suspected.
Should I pop the pimples from hot tub folliculitis
No, never pop or squeeze pustules from hot tub folliculitis. Manipulating the lesions can drive bacteria deeper into your skin, spread infection to surrounding follicles, and significantly increase your risk of permanent scarring. Let pustules heal naturally or with prescribed treatment. If they rupture on their own, gently clean the area with mild soap and water, then apply a thin layer of antibiotic ointment if recommended by your doctor.
Can you get hot tub folliculitis on your face or scalp
Yes, though it’s less common than on the trunk and limbs. Any area with hair follicles that was submerged in contaminated water can develop folliculitis, including your scalp, face, and hairline. Facial folliculitis deserves medical attention to minimize scarring risk and ensure proper treatment, as the skin on your face may require different management than body folliculitis.
Is hot tub folliculitis a sign of a dirty hot tub
Yes, almost always. Hot tub folliculitis indicates that Pseudomonas aeruginosa bacteria levels exceed safe thresholds, which only occurs when sanitizer levels are inadequate, pH balance is incorrect, or overall maintenance has been neglected. While “dirty” might suggest visible contamination, the problem is usually invisible water chemistry failure rather than obvious debris or cloudiness.
Will swimming in a chlorinated pool clear up hot tub folliculitis
No, this is a harmful myth. Swimming in a pool will not treat an existing skin infection and may actually worsen it, as the chemicals can irritate already inflamed skin. Hot tub folliculitis requires proper medical treatment or time for your immune system to clear the infection. Additionally, swimming in pools while you have active folliculitis is inconsiderate as you’ll introduce bacteria into that water.
Can I go in my hot tub if I have folliculitis
Absolutely not. You should avoid all hot tubs, pools, and communal bathing until your infection has completely cleared. Entering any body of water with active folliculitis can spread bacteria and potentially infect others. More importantly, the hot tub that caused your infection requires thorough decontamination through shocking, filter cleaning or replacement, and possibly complete draining before anyone uses it again.
What’s the difference between hot tub rash and hot tub lung
These are two entirely different conditions caused by microorganisms in poorly maintained hot tubs. Hot tub rash (folliculitis) is a bacterial skin infection from Pseudomonas aeruginosa that creates itchy pustules on your skin. Hot tub lung, medically called hypersensitivity pneumonitis, is a rare respiratory condition caused by inhaling aerosolized mycobacteria from contaminated water, leading to cough, shortness of breath, and flu-like symptoms. While both indicate serious maintenance problems, they affect different body systems and require different medical treatments.








