Table of Contents - Comprehensive Guide to Hot Tub Rash: Identification, Treatment, and Prevention
- What Is Hot Tub Rash
- Visual Identification and Differential Diagnosis
- Causes and Risk Factors
- Treating Hot Tub Rash
- Decontaminating Your Hot Tub Step by Step Guide
- Preventing Future Outbreaks
- Common Myths and Misconceptions
- Conclusion
- Frequently Asked Questions
- Is hot tub rash contagious from person to person?
- How long after hot tub exposure does the rash appear?
- Will hot tub rash go away on its own?
- Can I use my hot tub if I have a rash?
- Does chlorine kill the bacteria that causes hot tub rash?
- How do I know if my hot tub has the bacteria?
- Can I get hot tub rash from a bathtub?
- What is the best cream for hot tub rash?
This blog post may contain affiliate links. As an Amazon Associate I earn from qualifying purchases.
Hot Tub Rash Treatment: How to Heal Fast & Decontaminate Your Spa
Hot tub rash is more than just an inconvenient skin irritation that appears after a relaxing soak. Medically known as pseudomonas folliculitis, this bacterial infection affects thousands of hot tub users each year, turning what should be a therapeutic experience into an uncomfortable ordeal. This guide explores everything you need to know about identifying, treating, and preventing this common condition, while also addressing the crucial step many people overlook: properly decontaminating your hot tub to prevent reinfection.
Whether you’re dealing with an active outbreak or want to ensure your spa remains safe, understanding both the biological causes and the practical prevention strategies is essential. The Centers for Disease Control and Prevention (CDC) emphasizes that proper water chemistry and maintenance protocols are the foundation of preventing recreational water illnesses, and this article will walk you through every detail you need to maintain a healthy soaking environment.
What Is Hot Tub Rash
Hot tub rash represents a specific type of skin infection caused by exposure to contaminated water in spas, hot tubs, and heated pools. Understanding the underlying biology, recognizing the symptoms early, and knowing the typical timeline can help you respond quickly and effectively.
Medical Definition of Pseudomonas Folliculitis
Hot tub rash is caused by the bacterium Pseudomonas aeruginosa, an opportunistic pathogen that thrives in warm, moist environments. This organism is naturally present in many water sources, soil, and even on human skin, but it becomes problematic when it multiplies in poorly maintained hot tubs.
The warm water temperatures that make hot tubs relaxing (typically 100-104°F) create an ideal breeding ground for Pseudomonas. Heat causes your pores to open, making it easier for bacteria to enterhair follicles. Simultaneously, elevated temperatures accelerate the breakdown of chlorine and other sanitizers, reducing their effectiveness in killing bacteria.
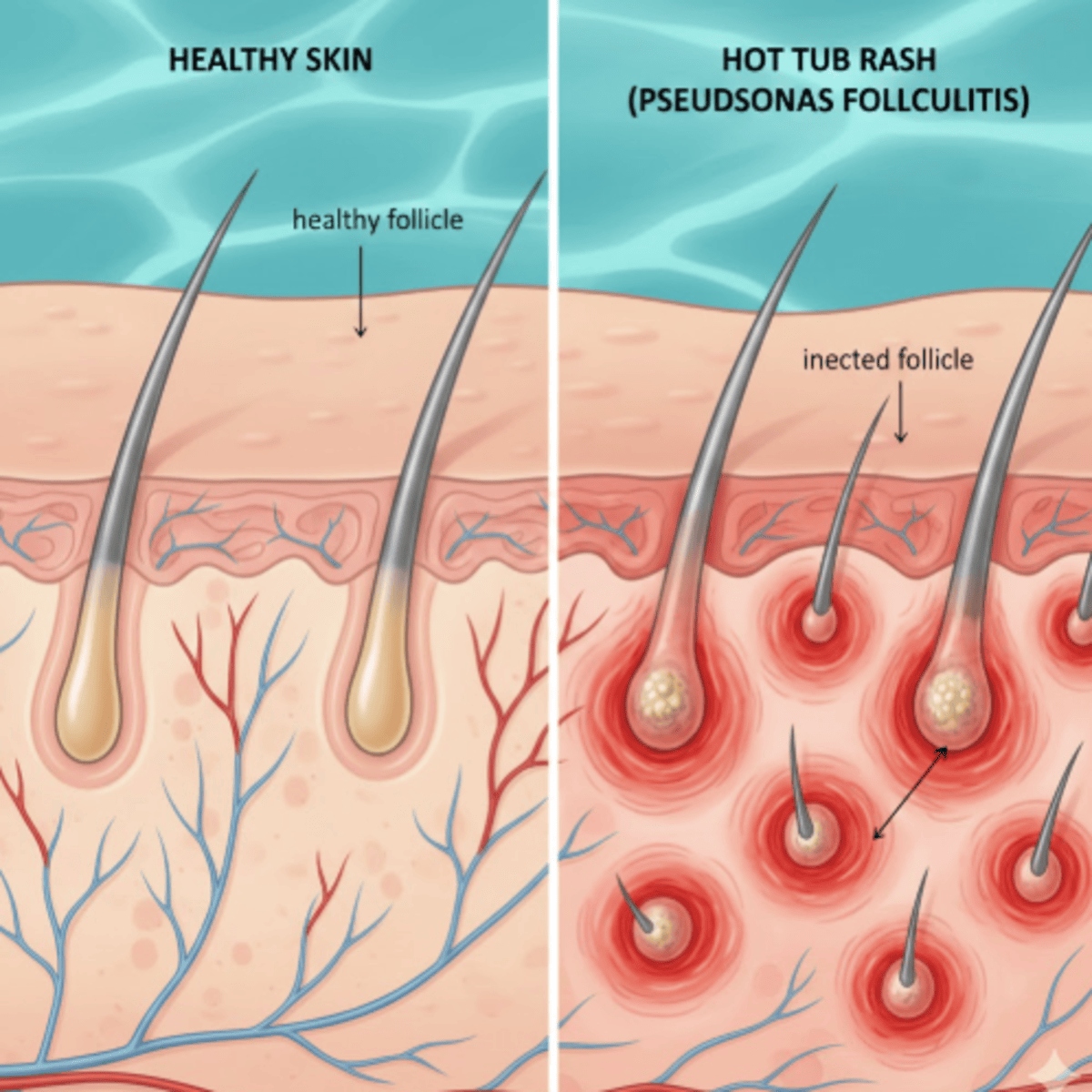
When contaminated water comes into contact with your skin, bacteria enter opened hair follicles and begin multiplying, triggering an inflammatory immune response. The result is an infection of the follicle itself, distinguishing this condition from simple skin surface irritation.
Identifying the Symptoms
The hallmark sign of hot tub rash is the appearance of red, itchy bumps scattered across areas that were submerged in the water. These bumps typically measure 2-10mm in diameter and may develop white or yellowish pus-filled centers, resembling small pimples or pustules.
The rash most commonly appears on skin that was covered by a swimsuit, particularly under the arms, on the chest, buttocks, and upper thighs. This pattern occurs because tight-fitting swimwear traps contaminated water against the skin for extended periods, giving bacteria more opportunity to penetrate follicles.
Beyond the visible skin changes, many people experience intense itching or tenderness in affected areas. The bumps may be sore to the touch and can spread if scratching introduces bacteria to additional follicles.
Some individuals develop additional symptoms including general fatigue, low-grade fever, sore throat, or earache. Ear infections can occur when contaminated water enters the ear canal, a condition sometimes called “swimmer’s ear” or hot tub ear, caused by the same bacteria.
The Incubation Period
One of the challenges in identifying the source of hot tub rash is the delay between exposure and symptom onset. Most people develop visible symptoms between 12 and 48 hours after using a contaminated hot tub.
This incubation period means you might not connect the rash to a specific hot tub session, especially if you use multiple water facilities or if several days pass before the outbreak. In some cases, symptoms can take up to five days to fully develop, further complicating identification.
The delayed presentation occurs because the bacteria need time to establish infection within the follicles and trigger a sufficient immune response to produce visible inflammation. Understanding this timeline is crucial for tracing the contamination source and preventing others from exposure.
Visual Identification and Differential Diagnosis
Accurately identifying hot tub rash requires distinguishing it from several similar-looking skin conditions. While medical diagnosis is always recommended for persistent or severe symptoms, understanding the visual characteristics helps you make informed decisions about seeking treatment.
What Does Hot Tub Rash Look Like

Hot tub rash typically begins as small red bumps that resemble goosebumps or a heat rash. Within 24-48 hours, these bumps may enlarge and develop into pustules with white or yellow centers, clearly indicating bacterial infection rather than simple irritation.
The distribution pattern is one of the most distinctive features. Unlike random bug bites or generalized allergic reactions, hot tub rash tends to cluster in areas where swimwear was tight or where water was trapped against the skin. You’ll often see the highest concentration of bumps under bra lines, waistbands, and along the edges of swim trunks.
As the infection progresses, individual bumps may grow to 5-10mm in diameter, sometimes forming small nodules beneath the skin surface. The surrounding skin often appears pink or inflamed, creating a halo effect around each affected follicle.
In severe cases, the pustules may rupture and crust over, leaving temporary dark spots or post-inflammatory hyperpigmentation that can persist for weeks or months after the infection clears.
Hot Tub Rash vs Chlorine Rash Chemical Dermatitis
Many people confuse hot tub rash with chlorine rash, but these are fundamentally different conditions requiring different responses. Chlorine rash, more accurately called irritant contact dermatitis, results from chemical exposure rather than bacterial infection.
Chlorine rash typically appears immediately or within a few hours of water exposure, whereas pseudomonas folliculitis develops 12-48 hours later. Chemical irritation causes dry, flaky, sometimes burning skin without the pustules characteristic of bacterial infection.
The location patterns also differ. Chlorine rash appears anywhere the chemical contacted your skin and tends to be more diffuse, while bacterial folliculitis concentrates in areas where swimwear trapped contaminated water.
Treatment approaches differ significantly. Chlorine irritation responds to moisturizers, cool compresses, and avoiding further chemical exposure, while bacterial infection may require antibiotics in severe cases.
Hot Tub Rash vs Bug Bites
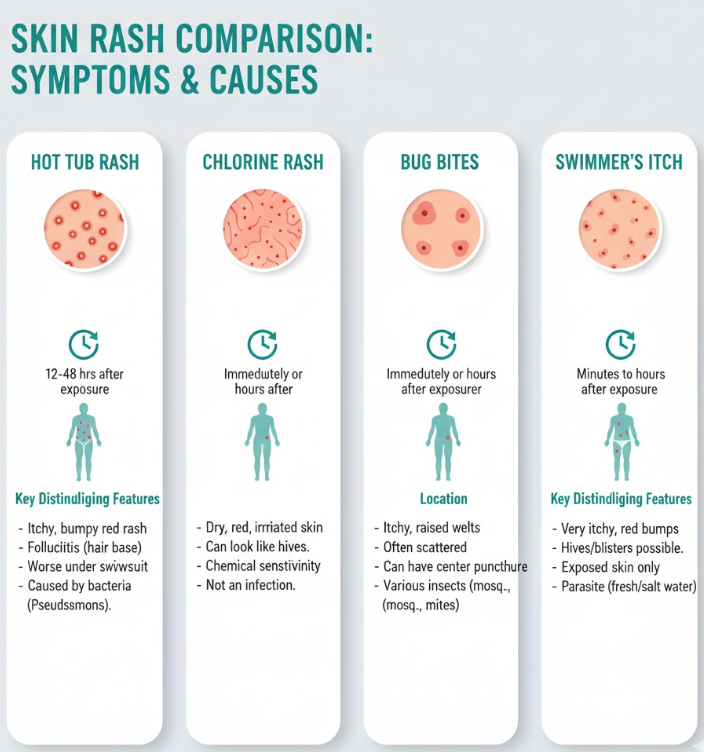
Insect bites can produce red, itchy bumps that superficially resemble folliculitis, but several key differences help distinguish them. Bug bites are typically larger, more scattered, and appear in random patterns rather than clustering under clothing lines.
Mosquito and other insect bites often develop within minutes to hours of exposure and are usually accompanied by localized swelling that extends beyond the bite site itself. They also tend to appear on exposed skin rather than covered areas.
Hot tub rash bumps are generally more uniform in size and appearance, while bug bites vary depending on the insect and individual reaction. Additionally, folliculitis bumps develop hair follicles at their centers, a detail visible upon close examination.
Hot Tub Rash vs Swimmer’s Itch
Swimmer’s itch, medically known as cercarial dermatitis, is caused by microscopic parasites that burrow into the skin in freshwater lakes and ponds. This condition differs significantly from the bacterial infection caused by hot tubs.
Swimmer’s itch typically occurs after swimming in natural bodies of water, particularly those frequented by waterfowl, whereas hot tub rash occurs in chemically treated heated water. The parasites causing swimmer’s itch cannot survive in properly chlorinated water.
The rash pattern also differs. Swimmer’s itch tends to appear on exposed skin areas not covered by swimwear, the opposite of hot tub rash distribution. The itching from swimmer’s itch is often more intense and begins as a prickling sensation immediately upon leaving the water.
Both conditions are self-limiting and resolve without treatment in most cases, but understanding the source helps prevent future exposures.
Causes and Risk Factors
Understanding why Pseudomonas aeruginosa thrives in spa environments and what factors increase infection risk empowers you to make informed decisions about hot tub use and maintenance.
Why Pseudomonas Aeruginosa Thrives in Spas
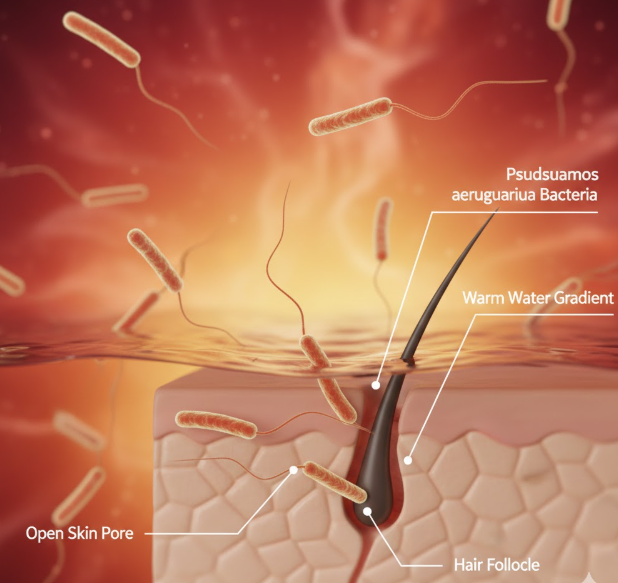
Pseudomonas aeruginosa is remarkably well-adapted to survive in aquatic environments, particularly the warm, aerated conditions found in hot tubs. The bacteria can tolerate a wide temperature range but multiply most rapidly between 95-115°F, precisely the range most spas maintain.
Heat degrades chlorine and other sanitizers more quickly than in cooler pool water. A hot tub maintained at 104°F may consume sanitizer three to five times faster than a pool at 78°F, creating windows of opportunity for bacterial growth between treatments.
The vigorous aeration from spa jets serves a dual purpose for bacteria. Bubbles and turbulence distribute organisms throughout the water, increasing contact with bathers, while also creating aerosols that can be inhaled or come into contact with face and eyes.
Organic matter from bathers including sweat, skin cells, lotions, and cosmetics provides nutrients that support bacterial growth. A single person entering a hot tub introduces millions of microorganisms and chemical compounds that stress the sanitation system.
The Role of Biofilm in Plumbing
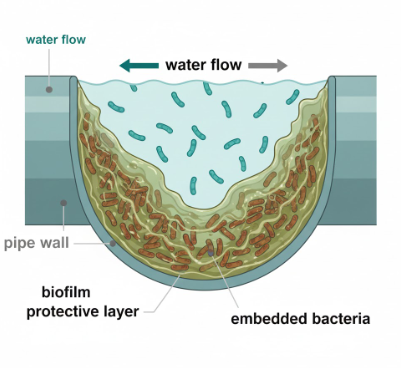
One of the most critical and often misunderstood aspects of hot tub contamination is biofilm formation within the plumbing system. Biofilm is a complex community of bacteria embedded in a protective slime layer that adheres to pipe walls, jet housings, and other surfaces.
Pseudomonas aeruginosa is particularly adept at forming biofilm, creating colonies that resist standard sanitizer levels. While free-floating bacteria in the water column may be killed by 3-5 ppm chlorine, bacteria protected within biofilm can survive concentrations ten times higher.
This protective matrix explains why a hot tub can have clear water, proper chemical readings, and still harbor the bacteria that causes folliculitis. The biofilm continuously sheds bacteria into the water, recontaminating the spa faster than sanitizers can eliminate the free-floating organisms.
Biofilm accumulates most readily in areas with low water flow, including the interior of filter cartridges, behind jets, and in dead-end plumbing runs. Once established, biofilm cannot be eliminated through routine shocking alone; it requires specific enzymatic cleaners or purging agents designed to break down the slime layer.
This is why proper hot tub maintenance goes far beyond simply adding chlorine. Those looking to invest in quality equipment should consider options from ONE HOT TUB, which offers models designed with improved circulation and filtration to minimize biofilm development.
Risk Factors for Bathers
While anyone can develop hot tub rash from exposure to contaminated water, certain factors increase susceptibility. Immunocompromised individuals, including those with diabetes, HIV, or undergoing chemotherapy, face higher infection risk and potentially more severe symptoms.
Children are particularly vulnerable for several reasons. They tend to spend longer periods in the water, increasing exposure time. Their immune systems are still developing, and they’re more likely to have microscopic skin abrasions from play that provide entry points for bacteria.
The duration of submersion directly correlates with infection risk. Each additional minute in contaminated water increases bacterial exposure and allows more organisms to penetrate opened follicles.
Tight-fitting swimwear, particularly in areas with elastic bands, traps contaminated water against the skin and creates the sustained contact needed for infection. This explains why the rash concentrates under swimsuit lines rather than on exposed skin that dries quickly after exiting the water.
Recent shaving or waxing creates microscopic cuts and irritation that compromises the skin’s protective barrier, allowing easier bacterial penetration. Using a hot tub within 24-48 hours of hair removal significantly increases folliculitis risk.
Treating Hot Tub Rash
Most cases of hot tub rash resolve without medical intervention, but appropriate home care can significantly reduce discomfort and speed healing. Understanding when professional treatment is necessary protects against complications.
Home Remedies and Self Care

The foundation of home treatment involves keeping affected areas clean and dry while managing symptoms. Gentle washing with antibacterial soap twice daily removes surface bacteria and prevents secondary infection from scratching.
White vinegar compresses provide effective relief for many people. The acetic acid in vinegar creates an environment less hospitable to Pseudomonas while soothing inflammation. Mix one part white vinegar with three parts clean water, soak a soft cloth in the solution, and apply to affected areas for 10-15 minutes several times daily.
Over-the-counter hydrocortisone cream (0.5-1%) reduces itching and inflammation when applied sparingly to affected areas. Avoid using strong steroid creams without medical supervision, as these can sometimes worsen bacterial infections by suppressing local immune function.
Calamine lotion offers cooling relief and helps dry weeping pustules. The mild astringent properties reduce oozing while the evaporative cooling effect soothes itching without the risks associated with scratching.
Resist the urge to pop or pick at pustules, as this introduces additional bacteria and increases scarring risk. If pustules rupture on their own, gently clean the area with mild soap and water, apply an antibacterial ointment, and cover with a clean bandage if needed to prevent spreading.
Proper hygiene for contaminated items is crucial. Wash all swimwear, towels, and clothing that contacted the contaminated water in hot water (at least 140°F) with detergent. Adding bleach (if fabric-safe) provides additional disinfection. Dry items on high heat to ensure any surviving bacteria are eliminated.
Avoid sharing towels, clothing, or personal care items during an active infection, even though person-to-person transmission is uncommon. This precaution prevents contaminating items that could theoretically reintroduce bacteria to your skin.
Medical Treatments
While most cases resolve without antibiotics, certain situations warrant professional medical evaluation. Seek medical attention if you develop fever above 100.4°F, if the rash spreads rapidly despite home care, or if you experience increasing pain, warmth, or red streaking from affected areas.
Severe pain, particularly if accompanied by swelling or hardening of the surrounding tissue, may indicate deeper infection requiring prescription antibiotics. People with diabetes, compromised immune systems, or other chronic health conditions should consult healthcare providers early rather than attempting extended self-treatment.
When antibiotics are necessary, fluoroquinolones like ciprofloxacin are typically first-line treatments, as Pseudomonas aeruginosa is often resistant to common antibiotics like amoxicillin or cephalexin. The bacteria’s resistance pattern means that standard antibiotics prescribed for other skin infections may be completely ineffective.
For severe or persistent cases, topical antibiotics such as silver sulfadiazine cream may be prescribed in addition to or instead of oral medications. This approach delivers high antibiotic concentrations directly to infected follicles while minimizing systemic side effects.
Some physicians prescribe gentamicin or tobramycin cream for localized treatment, particularly if oral antibiotics are contraindicated or if the infection hasn’t responded to initial treatment.
Never use leftover antibiotics from previous infections or antibiotics prescribed for someone else. Inappropriate antibiotic use contributes to resistance development and may delay effective treatment.
Recovery Timeline

Most people see improvement within 3-5 days of symptom onset, with complete resolution in 7-14 days without treatment. The timeline varies based on infection severity, immune system function, and whether medical treatment is utilized.
Itching typically subsides before visible lesions are completely clear. Pustules gradually dry and flatten, sometimes leaving temporary dark spots called post-inflammatory hyperpigmentation, especially in individuals with darker skin tones.
These dark spots are not scars but rather pigment changes that fade over weeks to months. Protecting affected areas from sun exposure during healing minimizes hyperpigmentation severity and duration. Using broad-spectrum sunscreen with SPF 30 or higher on healed areas helps prevent darkening.
True scarring from hot tub rash is uncommon unless infection was severe or lesions were repeatedly picked or scratched. Small pitted scars can develop from deep follicular infection, but these represent the exception rather than the rule.
If symptoms haven’t improved after two weeks of home care, or if new lesions continue appearing, medical evaluation is warranted to rule out alternative diagnoses or complications.
Decontaminating Your Hot Tub Step by Step Guide
Treating the rash addresses only half the problem. Without properly decontaminating the hot tub, reinfection is nearly guaranteed when you resume use. Standard shocking procedures are insufficient when biofilm contamination is present.
Why Shocking Isn’t Enough
Many hot tub owners mistakenly believe that simply adding extra chlorine or shock treatment will eliminate the bacteria causing folliculitis. While shocking does kill free-floating bacteria in the water, it cannot penetrate the biofilm matrix protecting bacterial colonies in the plumbing.
Biofilm acts as a physical and chemical barrier. The slime layer prevents sanitizer from reaching bacteria embedded within it, allowing them to survive even when the surrounding water contains sanitizer levels that would quickly kill unprotected organisms.
As soon as the shock level decreases through normal degradation, bacteria from the biofilm shed back into the water, recontaminating the spa within hours or days. This cycle explains why some hot tubs repeatedly cause infections despite owner efforts to maintain proper chemical levels.
Effective decontamination requires physical removal or disruption of biofilm before chemical sanitization can be fully effective. This multi-step process is more involved than routine maintenance but essential after a confirmed outbreak.
Step 1 The Biofilm Purge

Begin decontamination by using a specialized line-flush or biofilm removal product designed for hot tubs. Products like Ahh-Some, Spa Purge, or similar enzymatic cleaners break down the protective slime layer that harbors bacteria.
Follow the manufacturer’s instructions precisely, as concentration and contact time vary between products. Generally, you’ll add the purge product to the existing water (before draining) and run all jets on high for the recommended duration, typically 15-30 minutes.
During this process, you may see disturbing amounts of brown, gray, or greenish material floating in the water or expelled from jets. This material is the biofilm being dislodged from plumbing surfaces. While unpleasant to see, this confirms the process is working.
Pay special attention to running every jet configuration if your hot tub has multiple pump settings or diverter valves. Biofilm can hide in any section of plumbing that doesn’t receive regular flow.
Some stubborn biofilm may require a second treatment. If the first purge produces large amounts of material, drain the water, refill, and repeat the process until minimal debris appears.
Step 2 Drain and Scrub
After completing the biofilm purge, drain the hot tub completely. Don’t skip this step; the contaminated water contains the dislodged biofilm and millions of bacteria that must be removed.
Once empty, thoroughly scrub all interior surfaces including the shell, seats, pillows, and particularly the area just above the normal water line where biofilm often accumulates. Use a non-abrasive cleaner specifically designed for hot tub surfaces to avoid damaging the acrylic or fiberglass.
Remove headrests, pillow inserts, and any other removable components for separate cleaning. These items often harbor bacteria in seams and attachment points that regular water circulation doesn’t adequately sanitize.
Clean the cover interior thoroughly as well. The underside of hot tub covers stays warm and moist, creating ideal conditions for bacterial growth. Use a mild bleach solution (1 tablespoon bleach per gallon of water) or specialized cover cleaner, ensuring you rinse thoroughly afterward.
Don’t forget to clean the exterior cabinet access panels and any areas that may have been splashed during use. While these areas don’t directly contact bathers, maintaining overall cleanliness prevents cross-contamination.
Step 3 Filter Care
Filter cartridges deserve special attention during decontamination. The pleated material provides enormous surface area for biofilm development and traps organic debris that feeds bacterial growth.
After a confirmed Pseudomonas outbreak, the safest approach is replacing filters entirely. While this represents an additional expense, the risk of reintroducing bacteria from incompletely cleaned filters often outweighs the replacement cost.
If you choose to clean rather than replace filters, use a specialized filter degreaser and biofilm remover, not just a garden hose rinse. Soak filters in a filter cleaning solution or dilute bleach (1 cup bleach per 5 gallons water) for at least 8-12 hours.
After chemical soaking, rinse filters thoroughly with a high-pressure nozzle, spraying between each pleat to dislodge trapped debris. Any remaining biofilm will recontaminate your freshly cleaned hot tub.
Consider maintaining two sets of filters, rotating them during routine cleaning. This practice ensures you always have completely dry, clean filters available and extends the lifespan of each set.
Step 4 Refill and Superchlorination
After thorough cleaning, refill the hot tub with fresh water. Before allowing anyone to use the spa, perform a superchlorination treatment to eliminate any residual bacteria that survived the cleaning process.
Raise the free chlorine level to 10-20 ppm, significantly higher than the normal maintenance range of 3-5 ppm. Maintain this elevated level for at least 24 hours with the circulation system running continuously.
During this superchlorination period, keep the cover open to prevent chlorine gas buildup and accelerate degassing. The high chlorine level will naturally decrease through evaporation and UV degradation from sunlight.
Test the water several times during the 24-hour treatment period to ensure chlorine levels remain in the target range. Add additional sanitizer if levels drop below 10 ppm before the treatment period ends.
Before the hot tub is safe for use, test and balance all water chemistry parameters. Adjust pH to 7.2-7.8, total alkalinity to 80-120 ppm, and calcium hardness to 150-250 ppm. Proper water balance ensures sanitizers work effectively and prevents equipment damage.
Don’t allow anyone to enter the hot tub until free chlorine has dropped to the normal safe range of 3-5 ppm. Swimming in water with 10-20 ppm chlorine can cause eye irritation, skin irritation, and respiratory discomfort.
Preventing Future Outbreaks
Prevention requires consistent attention to water chemistry, bather hygiene, and regular maintenance. Establishing routine protocols significantly reduces infection risk while extending the life of your hot tub equipment.
Proper Water Chemistry Management

Understanding the difference between free chlorine and total chlorine is fundamental to maintaining safe water. Free chlorine represents the sanitizer available to kill bacteria, while combined chlorine (the difference between total and free chlorine) consists of spent chlorine bound to contaminants.
When combined chlorine exceeds 0.5 ppm, the water has high chloramine levels indicating sanitizer is being overwhelmed by contamination. This condition produces the characteristic “chlorine smell” many people mistakenly interpret as “too much chlorine” when it actually signals too little effective sanitizer.
Test water chemistry at least twice weekly during regular use, or daily during periods of heavy use. Use quality test strips or liquid drop test kits rather than relying on visual assessment. Clear water does not guarantee safe water.
Maintain free chlorine between 3-5 ppm for hot tubs, higher than the 1-3 ppm standard for pools. The elevated temperature and increased bather load per gallon in spas require more aggressive sanitization.
pH significantly affects sanitizer efficacy. Chlorine is most effective between pH 7.2-7.4. As pH rises toward 8.0, chlorine becomes progressively less effective, even if test readings show adequate ppm levels. At pH 8.0, chlorine is only about 20% as effective as it is at pH 7.0.
Total alkalinity acts as a pH buffer, preventing rapid fluctuations. Maintain alkalinity between 80-120 ppm to stabilize pH. When alkalinity is correct, pH becomes much easier to manage.
Test and adjust chemistry in the proper sequence: alkalinity first, then pH, then sanitizer. Attempting to adjust pH before correcting alkalinity often results in frustrating rebound where pH returns to the previous level within hours.
Bather Load and Hygiene
The single most effective prevention strategy many hot tub owners overlook is showering before entering the spa. A quick rinse removes the majority of lotions, cosmetics, deodorants, and body soil that feed bacterial growth and stress the sanitation system.
One study found that showering before pool or spa use reduces introduced contaminants by up to 70%. This simple step dramatically extends sanitizer effectiveness and reduces the frequency of water chemistry problems.
Establish a “no shower, no soak” household rule. While it may seem like an inconvenience, the one-minute rinse provides protection far exceeding the minor effort required.
Wash swimwear regularly, especially after hot tub use. Use detergent-free soap or specialized swimsuit cleaner, as regular laundry detergent contains phosphates and surfactants that create foam and introduce contaminants when the swimsuit is worn again.
Air-dry swimsuits completely between uses. Storing damp swimwear in plastic bags or closed spaces allows bacteria and mold growth that transfers back into the hot tub.
Limit the number of bathers and duration of use during each session. More people and longer sessions introduce exponentially more contaminants. A 15-minute soak for two people stresses the water far less than a 45-minute session with six people.
Avoid using the hot tub if you have open cuts, active infections, or diarrhea. These conditions introduce pathogens that contaminate water and put other users at risk.
Understanding proper maintenance is crucial for anyone considering alternative heating methods, such as those who use a Wood Fire Hot Tub, which may require different water treatment approaches due to the absence of automated sanitizer systems.
Routine Maintenance Schedule
Consistency prevents problems. Establish a maintenance calendar and adhere to it regardless of whether water appears clean or usage has been light.
Shock the hot tub weekly, even if test readings seem acceptable. Shocking oxidizes organic waste, breaks down chloramines, and provides a periodic boost to sanitizer levels. Use non-chlorine shock (potassium monopersulfate) or chlorine shock depending on your regular sanitization method.
Drain and refill the hot tub every 3-4 months under normal use conditions, or more frequently if the tub sees heavy use. No amount of chemical treatment can indefinitely maintain water quality as dissolved solids accumulate over time.
Before each refill, perform a line flush treatment to prevent biofilm accumulation. Making this part of your routine maintenance prevents the severe contamination that causes outbreaks.
Clean or replace filter cartridges monthly at minimum. Rinse filters weekly with a garden hose to remove surface debris, and perform deep chemical cleaning monthly. Replace filters annually or when the pleats become damaged or compressed.
Inspect and clean the cover monthly, particularly the underside. Wipe down with appropriate cleaner and allow to air dry before replacing. Well-maintained covers last significantly longer and reduce heat loss.
Keep detailed records of maintenance activities, chemical additions, and test results. This log helps identify patterns, troubleshoot recurring problems, and ensures you don’t skip scheduled tasks.
Common Myths and Misconceptions
Misinformation about hot tub safety and maintenance contributes to preventable outbreaks. Recognizing and correcting these misconceptions protects your health and your investment.
Myth Clear Water Means Clean Water
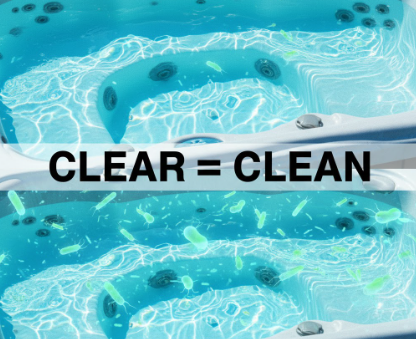
Perhaps the most dangerous misconception is that visually clear water indicates safe water. Clarity only indicates the absence of visible particles; it says nothing about dissolved contaminants, chemical balance, or bacterial load.
Pseudomonas aeruginosa is microscopic and completely invisible to the naked eye. Water can appear crystal clear while harboring millions of bacteria per milliliter. Biofilm can coat every surface of the plumbing system without affecting visual water clarity.
Relying on visual assessment rather than chemical testing puts every user at risk. The small cost and minimal effort of regular testing provides protection that no visual inspection can match.
This myth persists partly because proper sanitation often does produce clear water, creating a false correlation. The relationship works in only one direction: properly sanitized water is usually clear, but clear water is not necessarily properly sanitized.
Make testing a non-negotiable habit. Never assume water is safe based on appearance alone, regardless of how recently you added chemicals or how little the tub has been used.
Myth Saltwater Hot Tubs Can’t Get Rash
Some owners of saltwater hot tubs believe these systems provide immunity from folliculitis. This dangerous misconception stems from confusion about how saltwater systems actually work.
Saltwater hot tubs don’t use salt directly as a sanitizer. Instead, they use electrolysis to convert dissolved salt into chlorine, which then sanitizes the water. The end result is still chlorine sanitation, subject to all the same requirements for proper levels and water balance.
Saltwater systems can absolutely develop biofilm and harbor Pseudomonas aeruginosa if not properly maintained. The bacteria don’t distinguish between chlorine generated from salt electrolysis versus chlorine added from granules or tablets.
In fact, some saltwater systems may increase risk if owners assume the automatic generation means they don’t need to test and adjust chemistry regularly. Saltwater chlorine generators require proper water balance to function efficiently, and they can’t compensate for heavy bather loads or biofilm contamination.
Anyone with a saltwater system still needs to test chemistry regularly, shock weekly, clean filters, drain quarterly, and perform line flushes. The saltwater system simplifies routine chlorine addition but doesn’t eliminate any other maintenance requirements.
For those experiencing persistent issues despite maintaining chlorine levels, the problem may actually be Hot Tub Folliculitis caused by biofilm in the plumbing that standard sanitizer levels cannot penetrate.
Myth It’s Just a Heat Rash
Some people dismiss early symptoms as simple heat rash or prickly heat, delaying appropriate response. While hot environments can cause non-infectious heat rash (miliaria), the two conditions differ fundamentally.
Heat rash occurs when sweat ducts become blocked, trapping perspiration beneath the skin. It produces tiny, clear or red bumps that typically appear on clothed areas and resolves quickly once you cool down. Heat rash doesn’t produce pus-filled pustules.
Hot tub rash is an active bacterial infection that produces larger, inflamed pustules and doesn’t resolve simply by cooling down. The infection follows exposure to contaminated water, not just elevated temperature.
Mistaking folliculitis for heat rash can lead to continued hot tub use, spreading infection to others and potentially worsening your own condition. It may also delay appropriate treatment for more severe cases requiring medical intervention.
If bumps persist beyond 24-48 hours, contain pus, or worsen rather than improving after cooling, bacterial infection is far more likely than simple heat rash. When in doubt, consult a healthcare provider for accurate diagnosis.
Conclusion
Hot tub rash, while uncomfortable and frustrating, is largely preventable through proper maintenance and informed usage practices. Understanding that this condition results from bacterial infection rather than chemical imbalance or simple irritation is the first step toward effective prevention and treatment.
The dual approach of addressing both personal symptoms and environmental contamination ensures complete resolution. Treating the rash without decontaminating the hot tub leads to reinfection, while cleaning the tub without treating the infection leaves you uncomfortable during the recovery period.
Vigilant water chemistry management forms the foundation of prevention, but it must be paired with realistic expectations about what routine sanitization can accomplish. Biofilm formation in plumbing systems represents a persistent challenge that requires periodic deep cleaning beyond daily or weekly chemical maintenance.
Bather hygiene plays an equally critical role. The simple practice of showering before soaking dramatically reduces the contaminant load that overwhelms sanitizer systems and creates conditions favoring bacterial growth.
By committing to a consistent maintenance schedule, testing water chemistry regularly rather than relying on visual assessment, and responding promptly to any signs of contamination, you can enjoy your hot tub confidently while protecting yourself and other users from infection.
Remember that hot tub ownership carries responsibility not just for your own safety but for everyone who uses your spa. Taking these precautions seriously demonstrates respect for the health of family members, friends, and guests who trust that your hot tub is properly maintained.
With the knowledge and strategies outlined in this guide, you can maintain a clean, safe, and therapeutic hot tub environment that provides relaxation and health benefits without the risk of folliculitis or other recreational water illnesses.
Frequently Asked Questions
Is hot tub rash contagious from person to person?
No, hot tub rash is not contagious through direct person-to-person contact. The infection occurs when bacteria from contaminated water enter your hair follicles, not from touching someone who has the rash. However, sharing towels, swimwear, or personal items with someone who has been exposed to contaminated water should be avoided, as these items may transfer bacteria.
How long after hot tub exposure does the rash appear?
Symptoms typically develop between 12 and 48 hours after exposure to contaminated water. Some people may notice the first signs within 8 hours, while others might not see visible bumps for up to 5 days. This delayed onset can make it difficult to identify which hot tub caused the infection if you’ve used multiple facilities.
Will hot tub rash go away on its own?
Yes, mild to moderate cases usually resolve without medical treatment within 7 to 14 days. Your immune system typically clears the infection naturally while the skin heals. Using over-the-counter anti-itch creams and keeping the area clean can help manage discomfort during recovery. However, if symptoms worsen, spread rapidly, or you develop fever, medical evaluation is recommended.
Can I use my hot tub if I have a rash?
You should not use any hot tub until your rash has completely healed. Additionally, avoid using the specific hot tub that caused the infection until it has been properly decontaminated through draining, biofilm purging, and thorough sanitization. Returning to the contaminated tub will likely cause immediate reinfection.
Does chlorine kill the bacteria that causes hot tub rash?
Yes, chlorine effectively kills Pseudomonas aeruginosa when maintained at proper levels (3-5 ppm free chlorine for hot tubs) and when water pH is properly balanced (7.2-7.8). However, if bacteria have formed biofilm in the plumbing system, standard chlorine concentrations cannot penetrate the protective slime layer, allowing bacteria to survive and continuously recontaminate the water.
How do I know if my hot tub has the bacteria?
You cannot see bacteria without a microscope. Warning signs include cloudy water, a musty or “wet sock” odor, foam that doesn’t dissipate quickly, or sanitizer levels that drop to zero rapidly after adding chlorine. If someone develops folliculitis after using your tub, that confirms contamination. Professional water testing labs can perform bacterial cultures if you need definitive confirmation.
Can I get hot tub rash from a bathtub?
Standard bathtubs rarely cause this infection because water is drained after each use, preventing bacterial multiplication. However, jetted bathtubs with internal plumbing that retains water between uses can develop biofilm and harbor Pseudomonas aeruginosa. If you have a jetted tub, run the jets with a biofilm cleaner monthly and ensure the internal plumbing is properly sanitized.
What is the best cream for hot tub rash?
Over-the-counter hydrocortisone cream (1%) effectively reduces itching and inflammation for mild to moderate cases. Apply it sparingly to affected areas 2-3 times daily. For additional relief, calamine lotion can be used between hydrocortisone applications. Severe infections may require prescription topical antibiotics like silver sulfadiazine or gentamicin cream, which should only be used under medical supervision.